Biomechanics and Bioengineering of Orthopaedics: Component desingn
Hip and Knee Arthroplasty
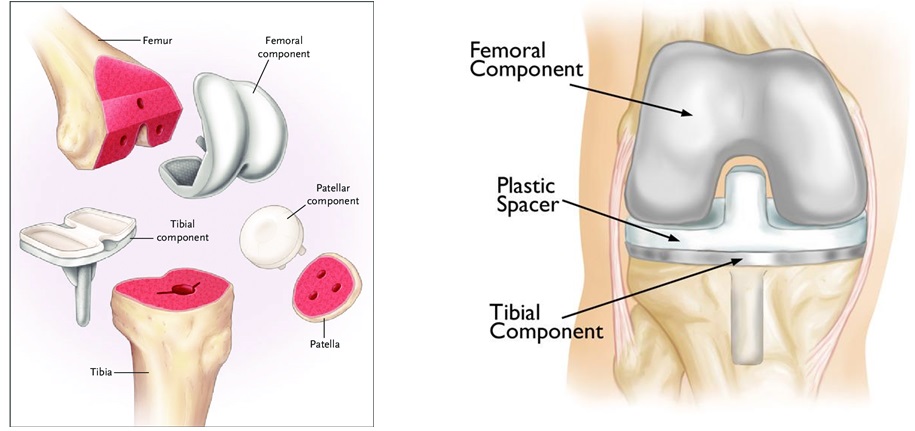
A total knee arthroplasty consists of four key components (Fig. 11-1):
The femoral component is a smooth metal piece with grooves imitating the femoral condyles that serves to resurface the worn lower end of the femur.
A plastic spacer imitates the natural cartilage and cushions the femoral component against the tibial component, reducing friction at the hinge.
The tibial component consists of a curved metal plate similar to that used for the femur. It resurfaces the worn portion of the upper tibia.
And finally, on the backside of the kneecap, a dome-shaped artificial ligament made of strong plastic is used to replace the patella.
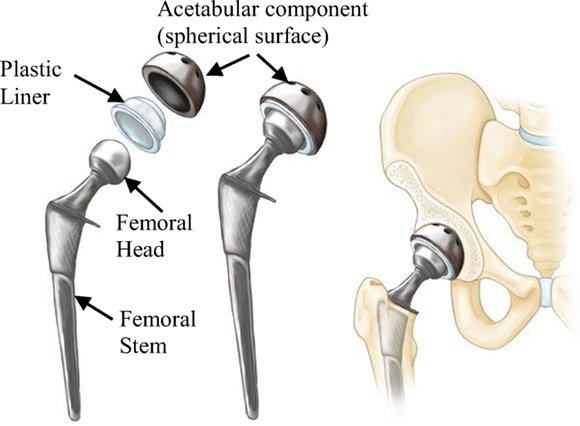
The key components of a hip prosthesis are (Fig. 11-2):
A metal acetabular shell fits inside the hip socket. Inside the shell is a plastic liner that functions as a weight-bearing interface; this layer must be both smooth and highly wear-resistant because of the chronic friction it experiences during user movement.
Next is the artificial femoral head which is fixed to the liner and caps the femoral stem. In a ball-and-socket joint, the femoral head is equivalent to the ball and is the center of the transverse, longitudinal, and sagittal axes about which the joint rotates. Inserted into the femoral medullary shaft is the femoral stem, which is a metal pin that stabilizes the prosthesis.
Implant Design (TKA)
For simplicity, the knee is considered a hinge joint because of its ability to bend and straighten like a hinged door. In reality, the knee is much more complex because the bone surfaces actually roll and glide as the knee bends.
Three different degrees of constraint are distinguishable in total knee replacement.
1. Non-constrained (bicruciate retaining, posterior cruciate retaining):
2. Semi-constrained (posterior stabilized, rotating hinged design)
3. Constrained (totally stabilized, hinged design)
In a non-constrained design (Fig. 11-3), knee kinematics is determined and guided by the ligaments. The femoral condyle articulates on a flat polyethylene liner. Either both the anterior and posterior cruciate ligaments or solely the posterior cruciate ligament is preserved. The mediolateral stability is given by the medial and lateral collateral ligaments. This implant may be appropriate for a patient whose PCL is healthy enough to continue stabilizing the knee joint.

In a posterior-stabilized design (Fig. 11-4), the cruciate ligaments are removed and parts of the implant substitute for the posterior cruciate ligament (PCL).

The total hinged design (Fig. 11-5) gives the highest constraint of knee motion; solely flexion and extension around a fixed axis in the sagittal plane is still possible. They are commonly used for revision surgery but can also help surgeons to improve implant stability in primary knee arthroplasty.

Mobile-Bearing vs. Fixed-Bearing Implants
Knee implants can also be classified as mobile-bearing or fixed-bearing (Fig. 11-6).
Fixed-Bearing Implants. In this design, the polyethylene of the tibial component is attached firmly to the metal implant beneath. The femoral component then rolls on this cushioned surface.
Mobile-Bearing Implants. In a mobile-bearing knee, also known as a rotating platform, the polyethylene insert can rotate short distances inside the metal tibial tray. This is designed to allow patients a few degrees of greater rotation to the medial and lateral sides of their knee.

Stems Design
The main purpose of using stems is to offload and reduce stress at the insufficient distal femur and proximal tibial bone.
Cementless stems are used in a hybrid technique having the tibial plateau cemented and leaving the stem uncemented. One major concern in using cementless stems seems to be the end to stem pain. Comparing the strain shielding of cemented and cementless stems, higher strain was found in cemented stems.
Short versus long stems
Biomechanical investigations have shown that longer and thicker stems reduce micromotion of the tibial tray. Shorter stems cause less peak stress according to finite element analysis.
Solid versus slotted stems
The stem-end design has been recognized to cause stem-end pain. It looks like the slotted stem causes less stem-end pain than the solid stem.
Key considerations in choice of material.
It is important to consider the similarity of the chosen material’s mechanical properties to that of the component’s anatomical counterpart. Example, making sure their modulus of elasticity is close enough to prevent stress shielding.
Also, consideration of the ultimate tensile strength of materials used for the acetabulum, femoral head, and femoral stem- must be greater than the upper-body loads transferred at the hip in order to prevent implant fracture.
We also need to consider the chosen material’s resistance to fatigue and fracture as well as wear resistance.
Currently, the most common materials used in hip and knee prostheses are metals such as titanium and cobalt-chromium alloys, ceramics such as alumina and zirconia, although more frequently composites of the two; and polymers such as U-H-M-W-P-E and high-crosslinked polyethylene.
Metals: Stainless Steel
Stainless steel is a common metallic alloy made from an iron-chromium mixture. Traditionally, biomedical devices using stainless steel also contained nickel, but nickel-free stainless steel has greatly improved corrosion resistance.
One type of low carbon stainless steel that is widely used in implants is 3-16 L stainless steel. Studies show that 3-16 L stainless steel has a yield strength of 190 Mega Pascal and ultimate tensile strength of 490MegaPascal, making it an ideal candidate for physiological load-bearing. With in vivo testing, stainless steel implants have been noted to “produce longer-term changes in blood composition”, particularly regarding the concentration of metal ions such as chromium and nickel.
Metals: Cobalt-Chromium Alloys
Cobalt-chromium alloys are an attractive alternative to stainless steel. Their increased wear resistance relative to stainless steel implants and significantly improved mechanical properties have made Cobalt-chromium alloys one of the most utilized materials for total hip and knee replacements. A common Cobalt-chromium alloy product, CoCrWNi (F90), has a yield strength higher than that of stainless steel at 310 Mega Pascal and an ultimate tensile strength of 860 Mega Pascal. It has been noted that long-term wearers of cobalt-chromium implants show elevated blood levels of metallic ions including hexavalent chromium, trivalent chromium, and cobalt ions, a mix of potential and known carcinogens.
Metals: Titanium Alloys
Titanium alloys are among the newer biomaterials on the market and have gained popularity due to their reduced weight and high mechanical strength. Newer titanium-based alloys, such as Ti33Zr5Fe4Cr, show a yield strength of over 1210 Mega Pascal and an ultimate tensile strength of 1711 Mega Pascal.
In terms of biocompatibility, titanium is more favorable than stainless steel or Cobalt-chromium implants since it displays only minimal release of metallic ions, leading many researchers to deem it a bioinert material.
Biomaterial scientists are able to enhance the biocompatibility and mechanical properties of titanium through surface modifications. Increasing the porosity of titanium alloys has been shown to stimulate bone growth in orthopedic implants and reduce the Young’s modulus to a more physiologically imitative range. Various surface modifications have been attempted to amplify the mechanical properties of titanium alloys, namely anodic oxidation and chemical vapor deposition, both of which aid in decreasing wear and corrosion of the material.
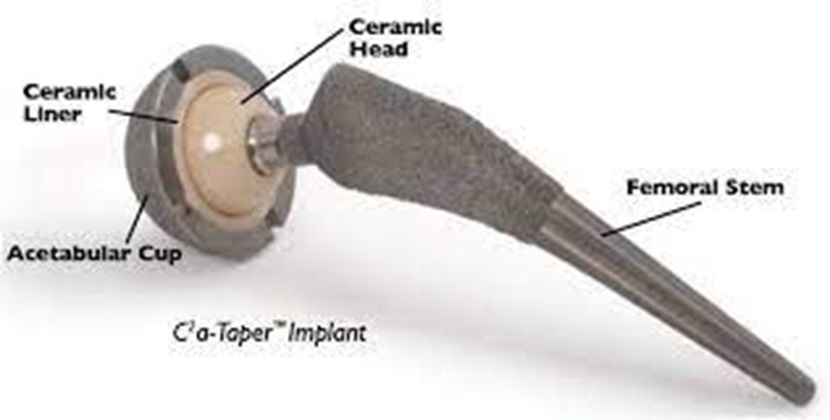
Ceramics
Ceramics are a unique class of biomaterials generally characterized by brittleness and rigidity (Fig. 11-7). Although early ceramics were simple ionic compounds containing a metal and a nonmetal, material scientists have maximized their mechanical advantages and created a new field of complex biomaterials to be studied. Today, many THA/TKA implants use ceramic-on-ceramic or ceramic-on-metal articulations to reduce corrosion due to wear.
Bioglass is a bioactive ceramic material largely composed of calcium, sodium and phosphorus. Bioglass is a suitable material for hard tissue replacement. bioglass and its derivative Novamin are commonly used as a coating for metallic bearings, as opposed to a bulk material. Due to its similarities to bone, bioglass shows excellent biocompatibility.
Alumina is another ceramic commonly used as a coating for metallic bearings in TKA/THA implants (Fig. 11-8). Since alumina is not very bioactive in orthopedic implants, it is often used in conjunction with a bioglass ceramic or zirconia to inhibit osteolysis. It is rare to find a pure alumina coating; however, even when applied as a thin film, alumina improves an implant’s mechanical properties, making it a desirable prosthetic material.
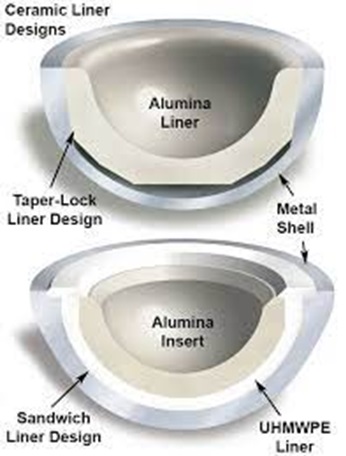
Like alumina, zirconia is rarely used by itself as a coating but rather is supplemented with bioglass, alumina, or a combination of the three. In comparison to alumina and bioglass, zirconia shows higher malleability and a lower ultimate tensile strength. Zirconia has the benefit of being more bioactive than alumina and often the two are used together in orthopedic implants to improve strength and biocompatibility (Fig. 11-9).

U-H-M-W-P-E is a polymer interface between harder ceramics or metals used for the acetabulum and femoral head. It exhibits hard-on-soft coupling, a beneficial phenomenon associated with reduced friction and wear at the interface.
Another common polymer in TKA/THA is PMMA, also termed bone cement, which is used to affix the femoral stem in the medullary cavity as well as repair small bone defects in revision TKA. Polyethylenes have evolved considerably with innovations in this decade aimed at improving wear resistance, such as antioxidant doping and gamma radiation-induced crosslinking.
